How DNA plays a role in Antibiotic Resistance?
Now more than ever bacteria are becoming pros at being resistant to antibiotics. Yet, how exactly does this occur? One major way would be by mutations. Mutations can occur in anything that has DNA, but in this instance, it would specifically be bacteria. Mutations happen in specific genes and whatever that gene produces can be targeted by antibiotics. For example, fluoroquinolones are a group of antibiotics whose target protein is an enzyme called DNA gyrase (helps to prevent coiling after DNA has been separated during replication). Now if a mutation occurs on the gene that produces DNA gyrase, the fluoroquinolones won’t be able to bind properly causing an excess growth of bacteria.
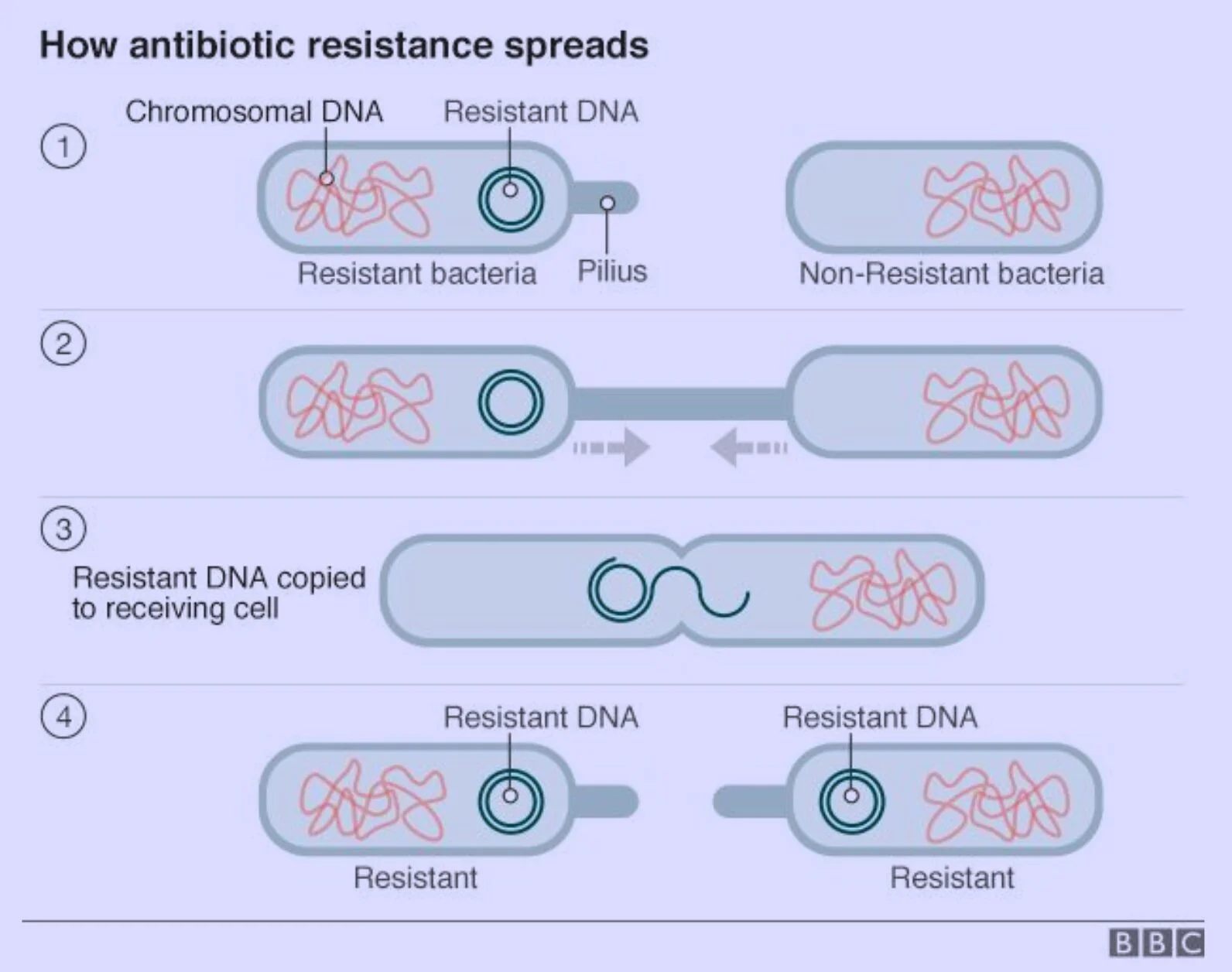
So that’s just one bacteria that has this mutation. How would that small event contribute to antibiotic resistance? Well, bacteria can exchange these mutations. There are three main ways of transportation: conjugation, transformation, and transduction. Conjugation occurs when two bacterial cells are close in proximity. When they are close a pilus (a long hair-like structure) is formed between them. The new resistant gene in their DNA replicates and goes into the other bacteria through the pilus. Transformation happens when a bacteria dies and the mutated DNA is released causing it to be free-floating. Another bacteria can salvage this DNA as its own. Lastly, transduction occurs when a bacteriophage (a virus) infects a bacteria taking up some of its DNA. This DNA may include the mutated gene. When the bacteria dies it will release the bacteriophage which will then go on to infect other bacteria. When infecting other bacteria it will take the previous DNA with it.
With all of this taking place, antibiotics are getting harder to administer each year due to the bacteria’s savvy techniques. While we can appreciate these cool techniques, they certainly don’t benefit us in the long run.
Picture Source: bbc.com